The Greek origin of the word diabetes means “to go through” or to “pass through.” Of course, this refers to excessive urine passing through the body during hyperglycemia (high blood sugar). However, I think “going through it” is a perfect way to sum up my experience living with T1D for the past 31 years.
An often-quoted statistic from a 2014 Stanford Medicine blog article (source) reported that people living with T1D make around 180 health-related decisions in a day. If this is an accurate estimate, I’ve made about 2,036,700 diabetes-related decisions in my life. Notably, these are not simple decisions. They are decisions that keep me cognitively and biologically functioning; these are decisions that keep me alive.
People living with diabetes are constantly performing what’s called “body listening” (source) and often monitoring our bodies in ways that others – including clinicians, nutritionists, and educators – do not fully understand if they do not live with it themselves. With every bite of food, every speaking engagement, every social interaction, we must constantly monitor our symptoms and be ready to correct our levels with insulin or sugar.
As a child, I recognized the way people’s behavior often changed after disclosing my diagnosis. In turn, I often hid it from people. I wanted to seem “normal,” and by hiding it, I was protecting myself from judgment and uneducated remarks about my diabetes management. I can’t count how many times I have been told to “take some insulin” when my sugar was already low or to “eat some sugar” when my sugar was already high. However, there are a lot of dangers in hiding it – including the danger of people thinking that I’m inebriated or disengaged when I’m, in fact, experiencing severe hypoglycemia and need to take a break. I did not feel comfortable making other people feel uncomfortable or dealing with the judgment that can come along with disclosure of a chronic illness like T1D. I was constantly negotiating which to sacrifice – autonomy over my decisions or my safety in case of a medical emergency.
It was not until I was older (and after plenty of therapy) that I was able to speak openly about living with this condition – including the negative parts. Once I was able to speak about it, I was able to fully address the connection between living with diabetes and my desire for perfectionism, the danger in striving for perfectionism, and the impact that others’ miseducation had on how I saw myself. It was also then that I was able to build a community with peers who live with T1D.

Examples of days I couldn’t seem to “get it right”
The most validating conversations I’ve had with peers were about the countless experiences we’ve had correcting well-intentioned, yet judgmental comments from people who do not live with T1D. We shared the grim realities of taking care of our T1D with depression and anxiety and how consistent low blood sugar increases suicidal ideation. We talked about feeling like a “failure” when we have a bad sugar day and the lack of motivation to continue monitoring because it felt like we will continually “fail” either way. We talked about the days when we just couldn’t get it right and wanted to give up.
This negative self-talk is a consequence and an internalization of societal judgment. These are not failures, and we do not have the option to give up. What we can do is give each other the space to talk about and validate the difficulties of managing T1D.
Prior to the availability of insulin to the masses in the early 1900s, patients living with “the sugar” were told to limit food intake and were essentially malnourished in attempt to avoid ketoacidosis and death (source). As most know now, T1D patients simply cannot survive without insulin. Thanks to monumental clinical and technological innovations, we have gradually gained more therapeutic options including fast-acting insulin, integrated blood glucose meters, continuous glucose monitors (CGM), insulin pumps, and more. No one can deny the fact that we must be grateful for the advancements that allow us to make better, more informed decisions. These technologies give many parents and caregivers relief knowing that their loved ones are safer. I often think about how terrifying it must have been for my mother to sleep at night knowing her 4-year-old daughter could experience life-threatening hypoglycemia throughout the night without a CGM to wake us up. It would be careless to say I am not grateful – I am incredibly grateful.

Little Kristy shortly after being
diagnosed with T1D
However, I hope people understand that gratitude and grief can coexist. We should still be able to speak about the challenges that exist.
The first time I saw a fitting depiction of both the physical and mental burden of T1D was when I watched The Human Trial documentary in 2023. I sobbed the first time I watched this documentary; I felt a deep connection with the people on the screen and knew that only we as patients and caregivers would understand this connection. As painful as it was, that connection also fueled me with an even stronger desire to fight for better treatments, and ultimately, a cure. It helped me realize that my anger about “toxic positivity” around diabetes was valid – that we, as a community, are grieving and often hiding how much we struggle because we are trying to be grateful for what we have at our disposal to manage this illness. It reminded me of the power of community, the power of authenticity, and how vital it is to have patients and caregivers create our own narratives – the good and bad.
As advocates, we must continue to tell our stories and participate in research when possible. As researchers, we must highlight what the high prevalence of diabetes distress means for our community (source): the need for a cure and continued clinical research on T1D.
For people looking to support someone with T1D in any capacity: I ask that you witness more and judge less. Stay curious. Do not make assumptions about how someone should manage their condition. It does not help. What does help us is more research, more funding, more inclusive language, and more patient leaders.
We are doing our best, and while we are doing our best, many of us are advocating for a world that better understands and supports us. Everyone can play a part in that by remembering that we are imperfect. Imperfection is a part of the human experience – even as diabetics. I am proud of all of us.
For more information and resources about patient-centered T1D perspectives and diabetes distress:
- The Human Trial documentary https://www.thehumantrial.com/
- Dangers of perfectionism https://beyondtype1.org/perfectionism-diabetes/
- Cognitive and psychological effects of living with type 1 diabetes: a narrative review https://pmc.ncbi.nlm.nih.gov/articles/PMC7154747/
- Janina Gaudin https://www.missdiabetes.com/
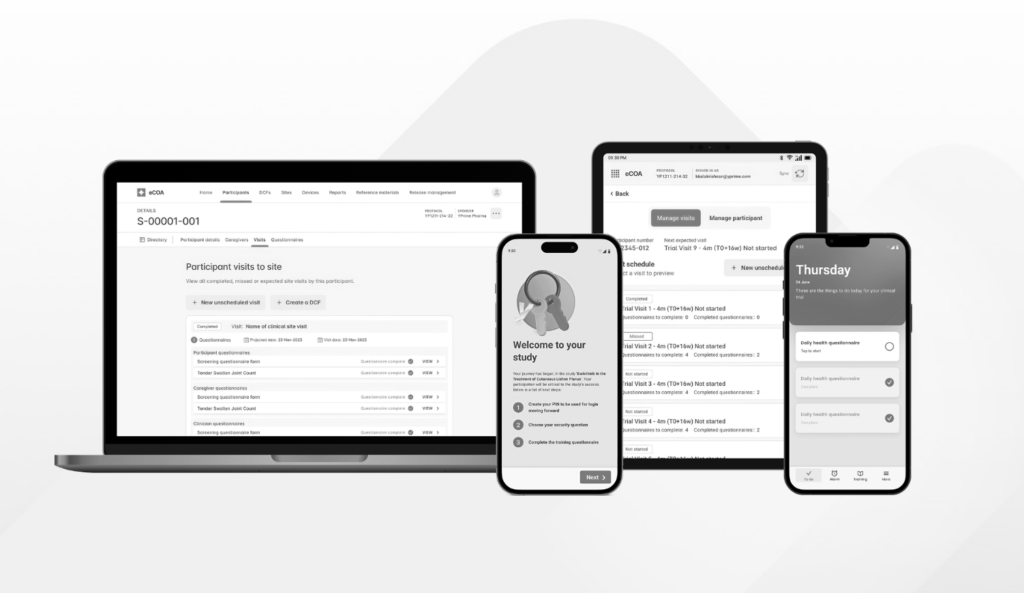
Check Out Our Other eCOA Resources
about trial design, data capture, operational efficiencies, and, ultimately, solving for certainty in clinical research.